Numerous conditions, such as strained muscles or ligaments, arthritis, or “pinched” nerves, can result in neck pain (when a nerve is irritated by something pressing on it). At any given time, 10% of adults experience neck pain. More women than men appear to be affected. Regardless of the cause, conservative therapy typically results in some of the pain relief. In this post we will try to understand some common causes of neck pain and understand meaning of these medical terms
Q What are the three types of neck pain?
Acute (lasting less than six weeks), subacute (lasting between six and twelve weeks), or chronic neck pain (lasting more than 12 weeks) are three categories of neck pain according to duration.
Q. Will my acute pain last for long?
While most acute pain episodes pass quickly, some people do continue to experience it in the long run.
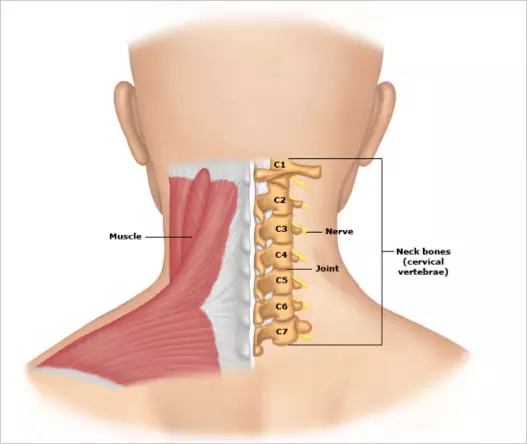
Q What is the normal framework of neck?
Seven square-shaped bones (cervical vertebrae), piled one on top of the other, make up the neck, or cervical spine. The names of the vertebrae correspond to where they are located in the neck, starting at the top with C1, C2, C3, and descending to C7. The skull can move thanks to a special connection between the upper cervical vertebrae and the skull. The cervical vertebrae work in concert with the surrounding long neck muscles and supporting ligaments to create a sturdy spinal canal that encases and safeguards the spinal cord.
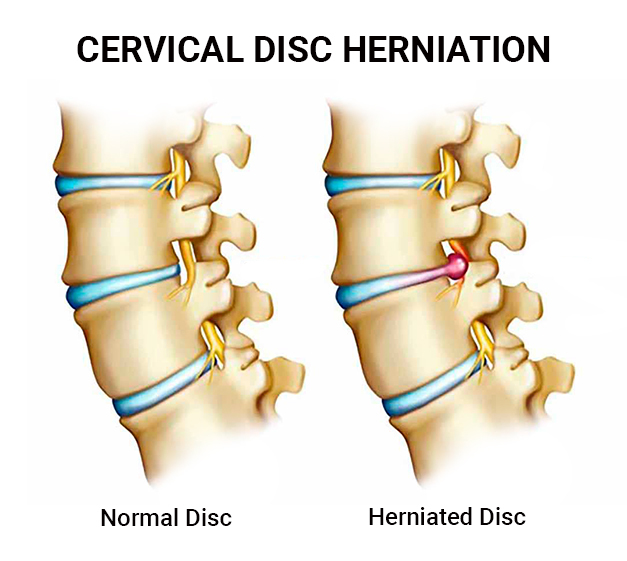
The discs, which act as shock absorbers and cushion the vertebrae between the neck bones, are located between the neck bones. A disc’s interior jelly-like material may protrude through its outer capsule if there is too much strain on it. A herniated or “slipped” disc is what this is. A herniated disc might result in symptoms if it irritates a nerve root. A disc issue may also be referred to as “bulging,” “protruding,” “extruded,” or “ruptured.”
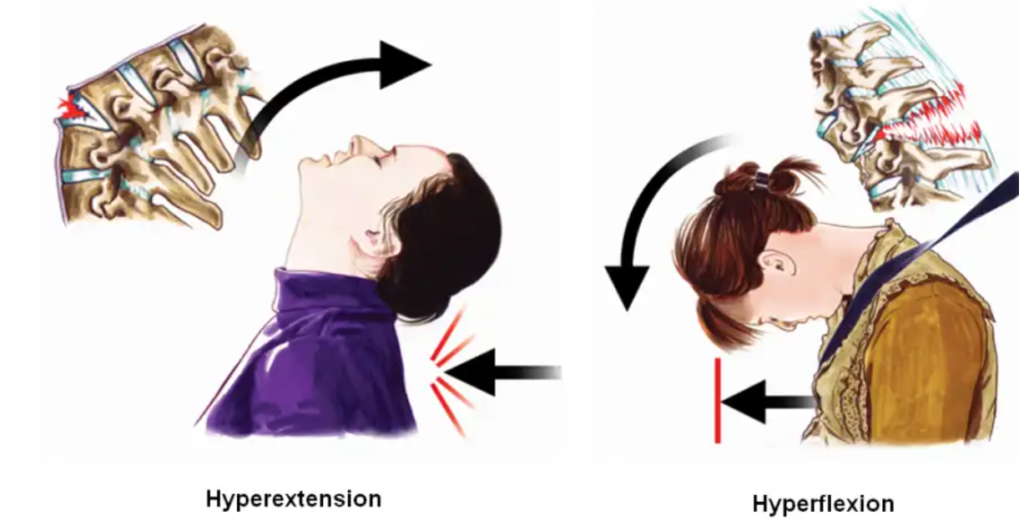
Discs and bones are directly covered by a thick layer of ligaments. The movement of the cervical vertebrae against one another is restricted by these dense tissues, which are intimately attached to the bones. These ligaments may get damaged as a result of head, neck, or upper body trauma or from car accidents. The intensity of this neck “whiplash” movement can range from moderate bruising to a full rip and separation of ligament from bone.
The neck’s main muscles make up the following layer of defence. These muscles hold the head up, keep the body in a neutral position, and support and move the neck. Neck strain or muscle tension are general terms used to describe overuse and discomfort of these muscles. These issues can occasionally be a factor in “muscle tension” headaches. Additionally, there are tiny muscles that attach in between the vertebrae and promote neck movement and posture.
Q How cervical strain causes neck pain?
A neck injury that results in a spasm (sudden tightness) of the cervical and upper back muscles might result in cervical muscular strain. The physical strains of daily life, such as bad posture, muscle tension brought on by psychological stress, or poor sleeping habits, can cause cervical strain. Cervical strain can also be brought on by sports-related injuries. The most common signs of a cervical strain are discomfort, stiffness, and tightness in the upper back or shoulder. These symptoms can linger for up to six weeks.

Q What is cervical spondylosis? What are its symptoms?
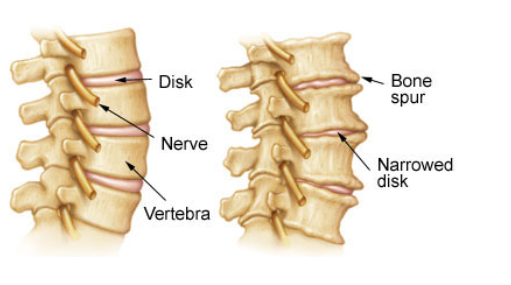
Degenerative changes in the cervical spine, also known as aberrant wear and tear, are the root cause of cervical spondylosis. As a result, the disc space gradually gets smaller, the natural square-shaped bone disappears, and bone spurs form (growths at the edges of the bones). These spurs may put more strain on the surrounding tissues and irritate nearby nerves. Normal ageing is expected to cause some wear and tear, but severe degenerative changes are uncommon.
Cervical spondylosis symptoms can include neck pain or weakness, numbness or strange feelings in the arms or shoulders, headaches, or restricted neck movement. In some situations, upper cervical spondylosis has also been linked to ear pain.
Q what is cervical discogenic pain?
The most frequent cause of neck pain may be discogenic pain in the cervical region. It results from degenerative alterations in the structure of one or more of the cervical intervertebral discs. Neck pain that worsens with head rotation or tilting is one of the common signs of discogenic pain. When the neck is held still for an extended amount of time, such when driving, reading, or using a computer, pain may become worse. Tightness and spasms of the muscles are frequently present. Additionally, transferred pain or strange feelings into the arm or shoulder may result from discogenic discomfort.

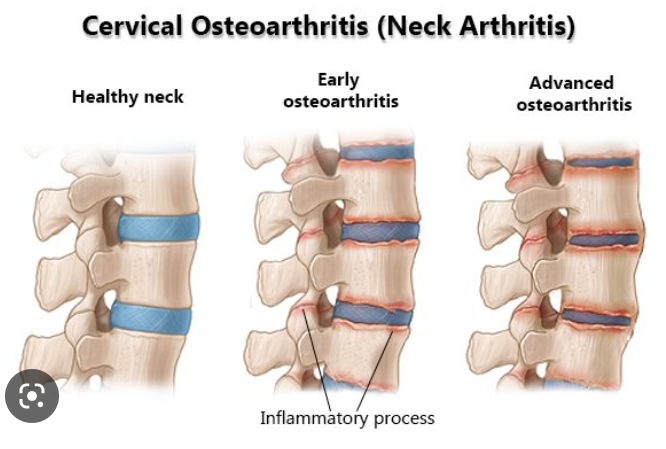
Q How cervical osteoarthritis causes neck pain?
The facet joints are located on sides of the vertebrae, and arthritis in this area can cause pain in the middle or side of the neck; some people also notice pain in the shoulders, around the shoulder blades, at the base of the head, into the ear and jaw, or in one arm. A common cause of pain due to cervical facet arthritis includes a job or other activity that requires repeated extension of the neck (tilting of the head backwards)
Q What is whiplash injury and how it results in neck pain?
The damage caused by a traumatic incident that causes a sudden forward/backward movement of the neck is referred to as “whiplash.” Accidents involving a motor vehicle are the most frequent cause of whiplash. When a large body blow occurs during a sporting event and the neck is required to control head motion, an injury of this nature may result. Numerous neck systems, including the muscles, ligaments, and joints, can be impacted by whiplash. Whiplash symptoms might include excruciating pain, muscle spasms, headaches, ear pain, jaw pain, and decreased neck mobility.
Q What is cervical myofascial pain?
Myofascial pain is a disorder that causes tight and tender areas of muscle that are sensitive to pressure. Myofascial pain in the neck can develop after trauma or can occur with other conditions, such as psychologic stress, anxiety, depression, or insomnia.
Q How cervical spondylotic myelopathy results in neck pain? What other symptoms it could have?
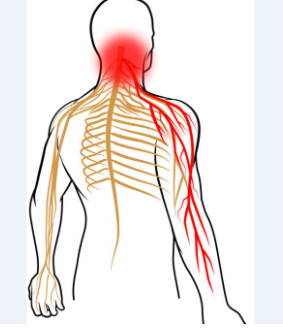
When the central spinal canal narrows due to degenerative changes, cervical spondylotic myelopathy develops. The cervical spinal cord may become injured or function incorrectly as a result of this constriction. Signs of cervical spondylotic myelopathy might include a number of neurologic problems in addition to pain and loss of mobility. Irritation of the spinal cord can lead to weakness, trouble walking or coordinating movement, inability to empty or control the bowels or bladder, and sexual dysfunction (erectile dysfunction).

Q What is cervical radiculopathy?
Cervical radiculopathy occurs when a nerve root is irritated by something pressing on it (a protruding disc, arthritis of the spine, or a mass or cyst). Symptoms of radiculopathy can include pain, weakness, or changes in sensation (such as numbness or tingling) in the arms.
To know more about this condition and discuss treatment options you can book appointment with doctor
- Note –This is a condensed summary of diagnostic, therapeutic, and medication information and is not intended to be exhaustive. It serves as a guide to aid in understanding potential diagnostic and treatment options and should not be considered a complete source of information. It does NOT encompass all details regarding conditions, treatments, medications, side effects, or potential risks that may be relevant to a particular individual. It is not a substitute for professional medical advice, which is based on a doctors assessment of a patient’s unique health status after examining them. To receive comprehensive information about their health, medical queries, and treatment options, including the risks and benefits of medication use, patients should consult a doctor. This information does not guarantee the safety, efficacy, or approval of any treatment or medication for a specific patient.