What is tension headache?
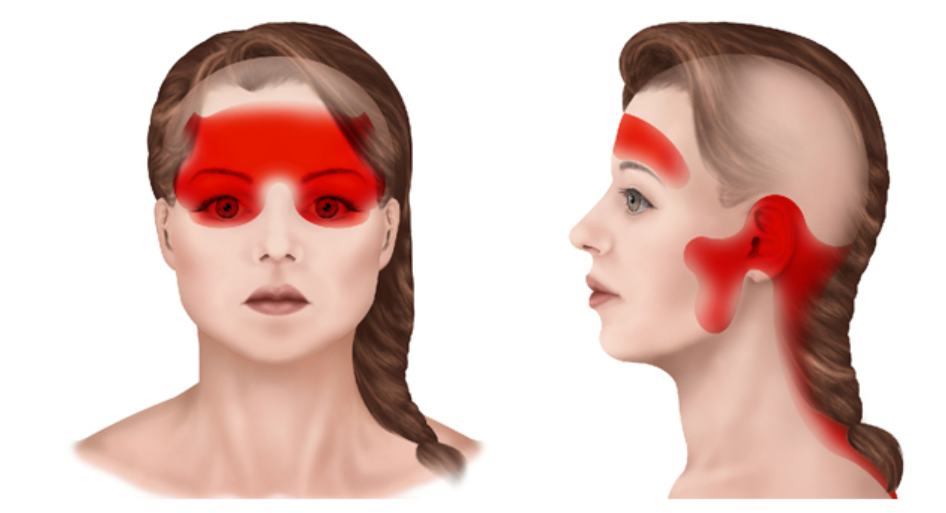
A tension headache is a tight, constricting pain that covers the majority of the head and is often brought on by stress or tension. It is also known as a tension-type headache or a muscle contraction headache. It is the most common form of headache. Two out of every three people will experience a tension headache at some point in their lives. Many sufferers do not realize that the headaches are associated with tension until it is pointed out to them. There may be tenderness in the muscles of the head, neck, or shoulders. Unlike migraines, tension-type headaches are usually not associated with other symptoms like nausea, vomiting, or sensitivity to sound or light.
What is the cause of tension headache?
Overactivity of muscles of the scalp, forehead and neck causes tension headache. A dull ache or tightness in these areas, like a tight band around the head or a heavy weight on top, results from this overactivity.
Trigger factors
• Increased tension or stress (both mental and physical),
for example:
––excessive worry
––all work—no play
––long periods of study, typing or other sustained concentration
––perfectionism
• Increased tension in the neck muscles, for example:
––poor posture
––injuries to the cervical spine (neck)
• Repressed hostility, anger or frustration
• A poor, scrappy diet, for example eating on the run
(combined with stress)
What is the treatment?
The key to treatment is to attend to lifestyle adjustments including diet, exercise, attention to posture of the neck and stress management.
Self-help
The best treatment is to modify your lifestyle in order to eliminate or reduce the trigger factors. For example:
• Learn to relax your mind and body.
• During an attack, relax by lying down in a hot bath or spa with a warm dry cloth (or even a cold wet cloth) over the aching area.
• You could attend special relaxation courses such as yoga or meditation classes.
• Be less of a perfectionist; do not be a slave to the clock.
• Do not bottle things up. Stop feeling guilty. Approve of yourself. Express yourself and your anger.
• If your neck is aching, massage or mobilisation followed by special exercises should help.
For more information on this topic visit http://drpiyushneurologist.com/neck-pain/
Medication
A mild painkiller such as ibuprofen or paracetamol can help stop the pain, but avoid stronger drugs (including tranquillisers) unless directed by your doctor. Mild pain relievers are also available in combination with caffeine, which enhances the medication’s effect; an example is acetaminophen, aspirin, and caffeine . This combination may be recommended if a pain reliever alone does not relieve the headache.
Am I using too many medicine for my headache? How to know and when to see a doctor?
Pain relievers should not be used too often because overuse can lead to medication-overuse headaches or chronic daily headaches. If your headache responds to a pain reliever, you should continue taking these with each headache. However:
●Do not use pain relievers more than nine days per month on average or more than two doses per episode.
●If a pain reliever does not control your headache, talk to your health care provider for other suggestions.
Why is doctor telling me to take medicines daily? What precaution should I take while taking these medicines?
Preventive therapy is recommended for people with tension-type headaches that are frequent or long lasting or have a significant impact on a person’s ability to do their normal activities.
Antidepressant medicines called tricyclics (TCAs) are often used to help prevent frequent tension headaches. Examples of TCAs include amitriptyline (used most commonly), nortriptyline, and protriptyline. The dose of TCAs used for people with headaches is typically much lower than that used for treating depression. It is believed that these drugs reduce pain perception when used in low doses, although it is not exactly clear how the medicines work.
It is common to feel tired when you start taking TCAs; this is not always an undesirable side effect since it can help improve sleep if you take TCAs in the evening. Your health care provider may recommend taking amitriptyline or nortriptyline two hours before bedtime to prevent morning grogginess. If morning grogginess occurs, then the medication could be taken even earlier (around dinnertime). TCAs are generally started in low doses and increased gradually. Their full effect may not be seen for weeks to months.
Is it possible to prevent tension headaches?
Yes, it is possible to prevent tension headaches by implementing the following strategies:
Practice stress management techniques: Find healthy ways to cope with stress, such as deep breathing, meditation, or yoga.
Maintain good posture: Keep your back straight, your head up, and your shoulders relaxed to prevent muscle tension in the neck and head.
Exercise regularly: Regular physical activity can help reduce stress and tension.
Get enough sleep: Aim for 7 to 9 hours of sleep each night and maintain a consistent sleep schedule.
Avoid triggers: Keep track of activities or circumstances that trigger headaches, and avoid or minimize them as much as possible.
Limit alcohol and caffeine: Excessive alcohol and caffeine intake can contribute to headaches, so it’s best to limit their consumption.
Stay hydrated: Drink plenty of water to avoid dehydration, which can cause headaches.
It’s important to note that everyone is different and what works for one person may not work for another. It may take some experimentation to find the best strategies for preventing tension headaches in your particular case.
Are there any home remedies for tension headaches?
Yes, here are some home remedies for tension headaches:
Practice relaxation techniques: Try deep breathing, meditation, or yoga to help relax the muscles and reduce stress.
Apply heat or cold: Use a warm towel or ice pack on the affected area to help relieve pain.
Massage: Gently massage the temples, neck, and shoulders to help release muscle tension.
Stay hydrated: Drink plenty of water to avoid dehydration, which can contribute to headaches.
Avoid triggers: Identify and avoid triggers such as lack of sleep, hunger, stress, and eye strain.
Exercise regularly: Regular physical activity can help reduce tension and stress.
Get enough sleep: Maintaining a consistent sleep schedule can help prevent tension headaches.
Note: If the headaches persist or worsen, it is recommended to consult a doctor.
When should a person see a doctor for a tension headache?
You should see a doctor if your headaches:
- Are frequent and interfere with your daily activities
- Are severe and last for an extended period of time
- Are accompanied by other symptoms such as fever, neck pain, vision changes, or confusion
- Are causing significant distress or affecting your quality of life
- Are not relieved by over-the-counter pain medication or home remedies
- Have started suddenly or have changed in pattern or intensity
- Are accompanied by other symptoms such as light sensitivity, nausea, or vomiting
If your headache is sudden, severe, or accompanied by other symptoms, seek medical attention right away, as these could be signs of a more serious condition. A doctor can help diagnose the cause of your headaches and recommend the best treatment plan.
Are tension headaches a chronic condition?
If headache is present for more than 15 days per month for at least three months then it is called chronic tension headache. For chronic tension-type headache, effective treatment involves the use of daily preventive medications (eg, tricyclic antidepressants), behavioral therapies, physical therapy, and lifestyle changes (eg, regular exercise and dietary changes).
To know more about this condition and discuss treatment options you can book appointment with doctor
- Note –This is a condensed summary of diagnostic, therapeutic, and medication information and is not intended to be exhaustive. It serves as a guide to aid in understanding potential diagnostic and treatment options and should not be considered a complete source of information. It does NOT encompass all details regarding conditions, treatments, medications, side effects, or potential risks that may be relevant to a particular individual. It is not a substitute for professional medical advice, which is based on a doctors assessment of a patient’s unique health status after examining them. To receive comprehensive information about their health, medical queries, and treatment options, including the risks and benefits of medication use, patients should consult a doctor. This information does not guarantee the safety, efficacy, or approval of any treatment or medication for a specific patient.